The U.S. Health System: An Overview
If you’ve ever felt like you're falling through the cracks of this poorly-knit system, that’s not just a feeling.
Hey there! If you’ve been enjoying this newsletter and finding value in the content, consider supporting my work by adding a paid subscription or donating through the Ko-Fi Link in my bio for coffee donations. Creating this takes time, research, and at least two cups of coffee per article—and paid subscribers help keep it all going. If my writing has informed, entertained, or saved you from a questionable Google rabbit hole, a subscription is a great way to say, “Hey, keep doing this.” Plus, you get the satisfaction of knowing you’re supporting independent work instead of, you know, another giant media conglomerate.
Thank you for taking the time to read my newsletter! I appreciate you being here!
Why It Feels So Disconnected
You (probably)- “Isn’t there just one healthcare system?”
Yes and no.
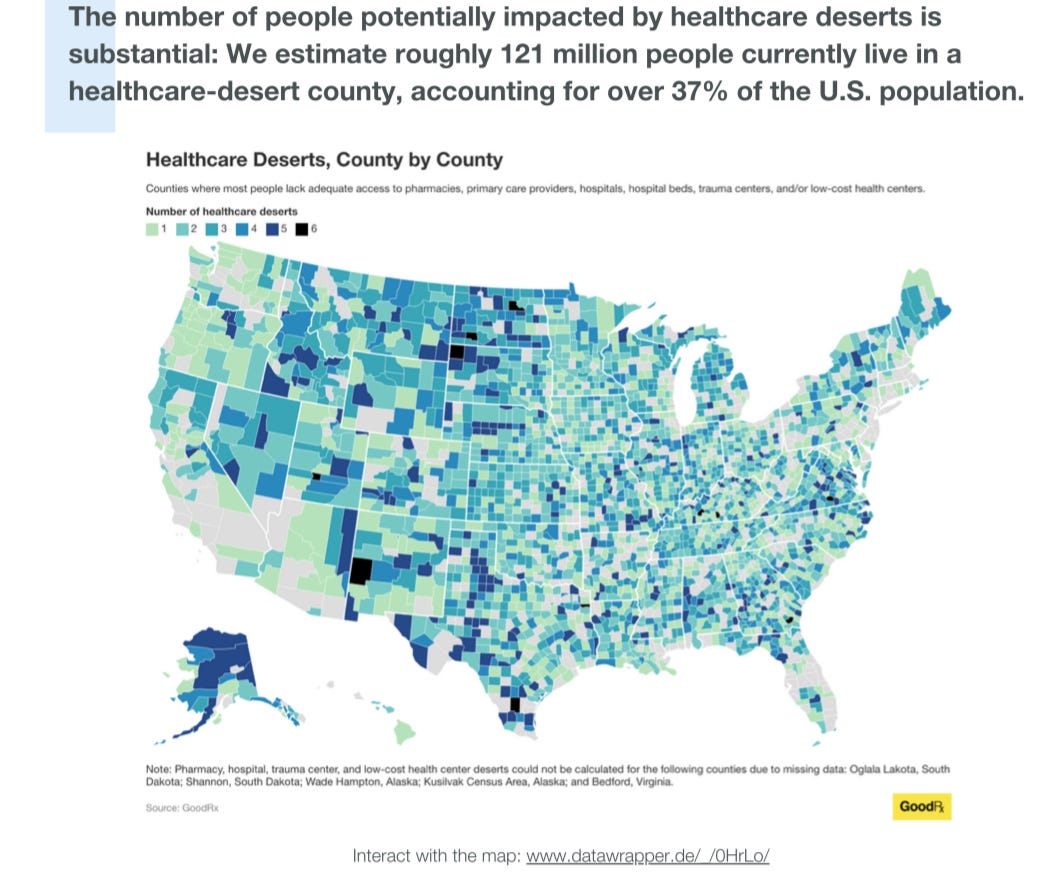
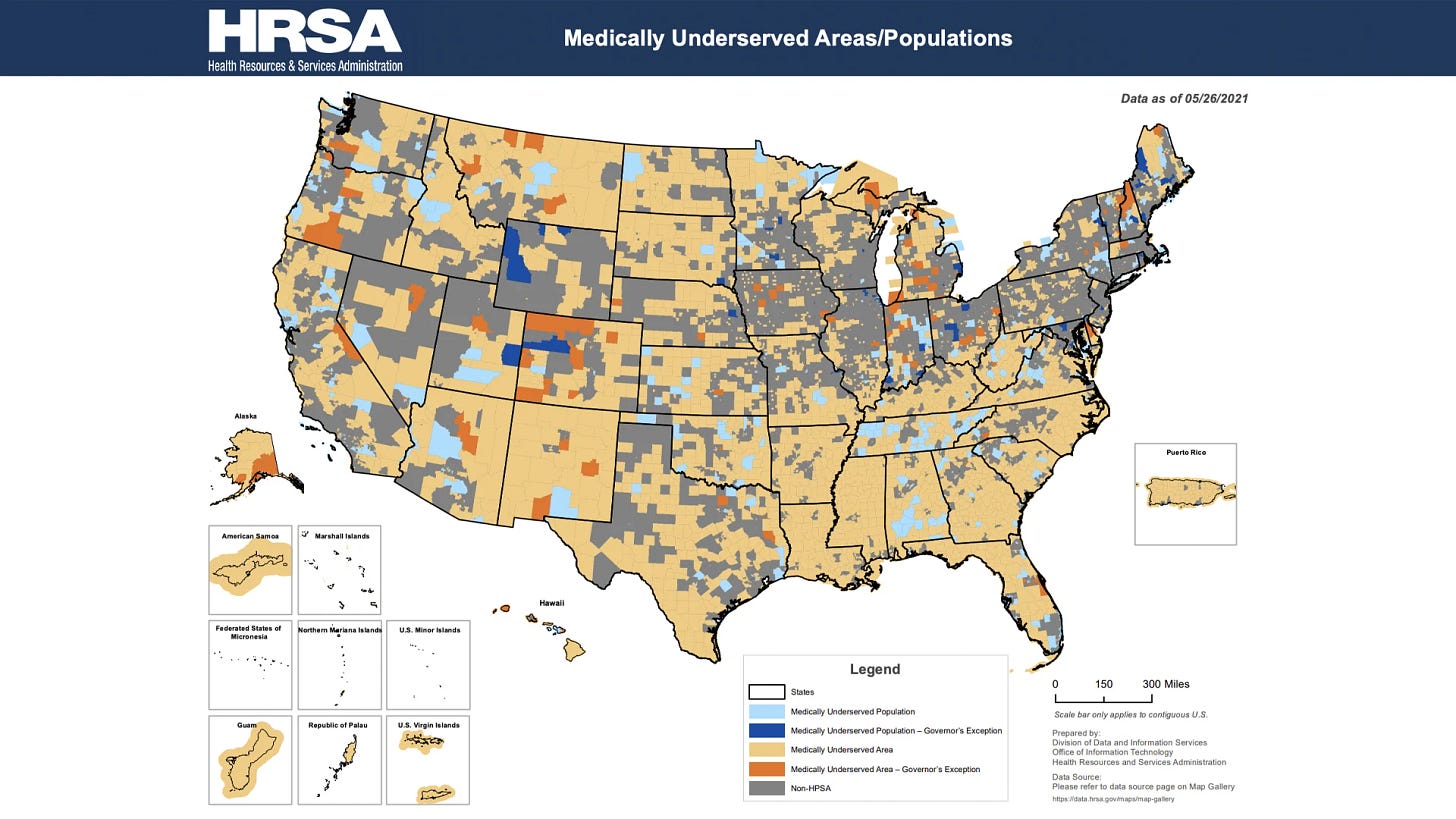
We don’t really have a singular healthcare system. We have a patchwork of systems—some public, some private, some charitable—that are loosely stitched together. So, if you’ve ever felt like you're falling through the cracks of this poorly-knit system, that’s not just a feeling. It’s, unfortunately, just how the system has come to exist.
This newsletter is a plain-language walk-through of how healthcare is set up in the U.S., how people move through it, and why it often feels chaotic or unfair.
The U.S. System Isn’t Really One System
Unlike countries with national health systems (like the UK or Canada), the U.S. system is built on a mix of public and private programs. That means:
There’s no universal healthcare
Where and how you get care depends on your job, income, age, military status, location, and even luck
Think of it like a messy kitchen where every family member is cooking their own meal, but using the same fridge.
The main systems include:
Employer-based insurance
Government programs (Medicare, Medicaid, VA, etc.)
Private insurance you buy yourself
Safety net & charity care
Public health services (like the health department)
AND, the icing on this cake is that none of them talk to each other very well.
How Most People Get Care (And What It Means)
If you’re working and insured through your job,
You likely have private insurance. Your employer pays part of the premium, and you pay the rest. You choose from a network of doctors.
If you're 65+, disabled, or have end-stage kidney disease,
You qualify for Medicare. It's a federal program with different parts (hospital, outpatient, drug coverage) that can be confusing to navigate.
If you're low-income or on disability,
You may qualify for Medicaid, run by your state with federal help. Coverage and rules vary a lot by state.
If you serve(d) in the military,
You might be eligible for VA healthcare or Tricare, depending on your service history.
If you buy insurance yourself,
You use the Marketplace (Healthcare.gov or your state exchange). You may get subsidies based on income.
If you’re uninsured,
You rely on:
Community health clinics
Emergency rooms (required to stabilize, not treat everything)
Public health departments
Safety net hospitals and charity care programs
The Public Health & Safety Net System
You might not think about public health unless there's an outbreak, but it's a critical piece of the U.S. healthcare puzzle.
Public health departments handle:
Vaccinations
STD testing and treatment
Disease surveillance
Environmental health (like lead or water safety)
Emergency preparedness
These services are usually free or low-cost but often underfunded and overstretched.
The Safety Net includes:
Federally Qualified Health Centers (FQHCs)
County or public hospitals
Free clinics
Planned Parenthood
Mobile units or community outreach programs
These places help people who:
Are uninsured
Are undocumented
Can’t afford private care
Face barriers due to language, transportation, or stigma
“The safety net isn’t extra — for millions, it’s the only net keeping them from hitting the ground.”
Here’s one of the many catches: the safety net is not universal or guaranteed. It’s a patchwork (like we discussed above), and it varies drastically by city and state.
Why It All Feels Disconnected
In the U.S. system:
Your primary care doctor might be part of one network
Your specialist might be part of another
Your insurance might only approve certain drugs
Public health and primary care are funded by different budgets
Mental health is often carved out and handled separately
There's no centralized coordination. That’s why:
You fill out the same forms over and over
You have to explain your medical history 10 times
Nobody seems to “have your file”
You’re the one keeping track of everything
Real Talk:
The U.S. healthcare system was built to prioritize access to services — not continuity of care— (which is funny…not really) because most of the time, it feels inaccessible. So, in many cases, they’re there, but they’re also not. Make sense?
That means you can usually find someone to treat you, but making it make sense is another story.
The Challenges of a Disconnected System
When systems don’t talk to each other, patients pay the price, and not just financially—emotionally, physically, and logistically.
Here’s what that disconnection looks like in practice:
Redundant tests and procedures
You might get the same lab work done multiple times because one provider can’t see the results from another.Gaps in care
When there’s no smooth hand-off between providers, things fall through the cracks—medications get missed, follow-ups don’t happen, and symptoms get overlooked.Confusing medical bills
One visit could generate multiple bills: from the hospital, a specialist, a lab, and a separate billing company. And good luck figuring out who to call with a question.Delayed diagnoses and treatments
Providers often don’t have access to your full medical history, which slows down decision-making or leads to poor decisions based on incomplete info.Mental health fragmentation
Behavioral health is often handled separately, with different networks, providers, and rules. It makes coordination with your primary care provider extremely difficult.Lost time and trust
Patients spend hours navigating phone trees, hunting down records, rescheduling due to “insurance issues,” or just trying to figure out where to go next.
All of this leads to a system that is hard to trust, harder to navigate, and deeply inequitable. The burden of making it work falls disproportionately on patients, especially those already dealing with chronic illness, language barriers, disabilities, or economic stress.
I don’t like the excuse that “this is just how things are.”
It’s the result of policy decisions, industry structures, and a lack of coordination that prioritize access to services over access to care.
Why Understanding This Helps You
When you understand how the U.S. system is structured, you can:
Navigate care more confidently
Ask better questions (“Is this doctor in my plan’s network?”)
Know where to go when something goes wrong
Avoid scams, misinformation, or redundant care
Advocate for better policies that actually fix the system
This knowledge doesn’t fix the flaws, but it gives you tools to move through them with more power, not just frustration.
Call to Action
Have you ever fallen through the cracks of this “system”? Have you ever felt like nobody in healthcare is talking to each other?
Reply or comment: I’d love to highlight your story.
If this helped you understand how it all fits together (or doesn’t), please share it with a friend or family member who’s trying to figure it out too.
Until next time,
Caroline Waltzman
Your health Translator and Navigator, one newsletter at a time





Thanks, Caroline. Great overview. I'm an ER physician. We need so many more of us that think in systems. We can't effectively transform what we don't understand.